In the blog post Understanding Attachment Reminders – Part 1, you learned that Dentrix Ascend has automated attachment reminders that help you know exactly what each insurance carrier requires for specific procedures when you are submitting insurance pre-determinations and insurance claims.
So, you may be wondering, “How will I know if the attachment requirements are up to date?” or “What if the insurance carrier changes their attachment requirements?”.
We understand your concerns. Dentrix Ascend will automatically update insurance carrier attachment requirements as mandated by each insurance carrier. That means you can focus on processing insurance claims and pre-determination so you can take care of your patients’ treatment needs. No action is required on your part.
Additional Information
- To learn more about insurance claim and pre-determination attachment reminders, read Understanding Attachment Reminders – Part 1 in the #DentrixAscendBlog.
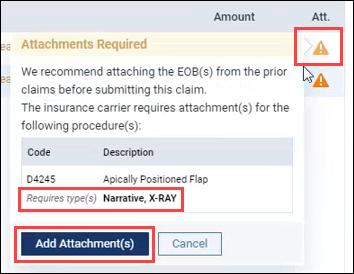
- There is no option to turn off this warning notification feature.
- In cases where a secondary insurance claim needs an attachment, the warning message includes a recommendation to attach the EOB(s) from prior claims before submitting the claim.
- To learn more about how to add attachments to claims, watch Adding Attachments to Claims in the Dentrix Ascend Resource Center.
